A telltale sign that who you’re evaluating isn’t a leading mental health clearinghouse is if they don’t have experience integrating with the EHR your organization’s using. You see, MCOs are usually still large insurance payers, making it hard to get through to them regarding a specific claim from one of your clients. So, your clearinghouse should have direct contacts to reach out to on your behalf regarding any issues with your https://www.bookstime.com/articles/what-is-a-bookkeeper claims. Your clearinghouse should be able to help with the denial recovery process by explaining what happened, pointing out errors, and generating appeals letters or resubmitting corrections to payers. Health insurance organizations don’t make this entire process easy, but they have their rules. Before you “officially” send your claims to your client’s payers your clearinghouse should help you out via scrubbing and rejections.
SOAP Notes PDF Template for Mental Health Providers
Diagnosis coding allows mental health professionals to identify different treatments, diagnoses or actions given to the patient. Diagnosis coding is documented to make it easier to categorize different mental disorders or diagnostic evaluations during therapy. Insurance companies need to see that the patient has a clear diagnosis that is mental health billing for dummies medically necessary and qualifiable for covered mental health insurance. Everything transpiring between a patient and the mental healthcare provider should be in the medical record. A patient’s medical record determines what is billed for the mental health service, which means that all required information must be adequately documented.
Claim ID or Claim Number for Corrected Claims
Many clearinghouse solution providers will ask you what EHR your organization utilizes during initial deliberations. They should have features included within it that I also included within the terms section from earlier as well such as; rejections, claim scrubbing and denial management. Your clearinghouse should also keep a record of your denials and place them within work queues to kick off the appeal process.
- Although troubling, receiving a denial from a payer for a claim you submitted isn’t the end of the world.
- You will generate more demand and less billing reputation than other medical services.
- IF YOU MUST bill claims via paper, ask about their claims address as well.
- Mental health CPT code modifiers can describe the way services are rendered as well, telehealth modifiers as an example.
- Apart from the confusing ICD Codes with CPT code assignment errors, the other kind of mistakes that could occur include undercoding or upcoding.
CPT Codes and Modifiers for Mental Health Claims
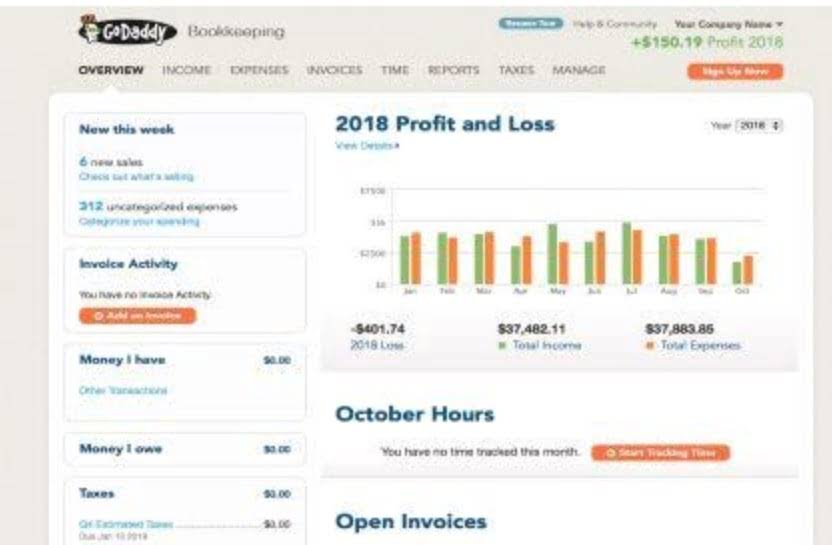
The tools you use to handle the revenue cycle can make billing more manageable. Unless you outsource all billing to a third party, you should arm yourself with tech and reporting capabilities that smooth the process and position you for success. Good billing practices begin the moment you initiate a new patient record. Remember way back in step 2 when I mentioned the phone call to the number on the back of your client’s insurance card? If ALL of your patients had Health First Colorado as their payer, this wouldn’t be that bad of a manual process…but that’s not the case. The image above is a screenshot of Health First Colorado’s claim submission web portal.
Complete Guide to Mental Health Billing
- This includes deductibles, co-payments, coinsurance, or any services not covered by the insurance plan.
- We have a guide called “How to Check Mental Health Eligibility and Benefits” at this link which contains a script and thorough questions to ask so you gather all necessary information.
- They can also identify related health problems and are used with CPT codes for billing insurance.
- These codes help identify and bill for specific mental health interventions, such as individual therapy, group therapy, or medication management.
- POS codes identify the physical location where a healthcare service is provided.
- Speak with an insurance representative directly for ideas on how to fix and resubmit denied requests.
- In short, you’ll receive more money and avoid unpleasant surprises by getting the copay out of the way up front.
CPT codes are a standardized set of codes maintained by the American Medical Association (AMA). These codes are used to identify specific procedures and services provided by healthcare professionals, including mental health practitioners. Integrated practice management systems can help you auto-generate bills with correct formatting and accurate data. For example, software that generates automatic claims after appointments will make your job easier than software that requires providers to initiate every claim.

- Moreover, when you work with experts, there are fewer chances of errors because experts know how to deal with these insurance companies.
- The digital systems have been really kind to us with the new advancements.
- You can work hard to submit your claims, and go above and beyond for it as well.
- Refer to the table below to find the correct license level modifier to use when coding modifiers for your behavioral health insurance claims.
- Sometimes the patient’s plan simply doesn’t cover a particular treatment and there’s little you can do.
- Include the client’s demographic and insurance information, diagnosis codes (ICD-10 codes), procedure codes (CPT codes), and any necessary modifiers.
To get paid for their rendered services, they need to follow some complex procedures of medical billing services. Once the insurance company processes the claim, you will receive an Explanation of Benefits (EOB). Review the EOB to ensure accurate payment and check for any denials or adjustments. If a claim is denied, identify the reason and take appropriate action to correct and resubmit the claim promptly. This may involve providing additional documentation or appealing the denial if necessary. A clean claim is formatted correctly, contains accurate information, and is free of mistakes or typos.
Clearinghouse
How to Bill for Mental Health Services: A Beginner’s Guide
- You have all the necessary patient and session information to file claims.
- Every insurance payer has a series of requirements required to receive reimbursement for claims.
- Ensure clear communication about payment due dates, accepted payment methods, and any applicable late fees or collection policies.
- Therefore, it is important for everyone to understand what mental healthcare billing is right from its basics.
- If you mention the word “billing” to any mental professional, they’ll shutter.
- Different modifier codes are used to tell the extra information to payers about the patients’ treatment.
- Once scrubbed, your claim is ready for submission to a payer for reimbursement.

Commentaires récents